Fatigue is very common with many Neurological and long-term conditions and is one of the most frequently reported symptoms in MS. We all experience physical and mental tiredness as part of our normal daily lives; however fatigue can feel very different from the normal sensation of tiredness. People living with MS describe fatigue as an “overwhelming tiredness” or a “sudden loss of energy,” often for no apparent reason.
Fatigue can limit or affect the ability to complete essential daily activities, such as getting dressed, going to work or walking the dog. Additionally, it might affect your thinking processes, speech, physical movements, or a combination of these. Some patients living with MS, additionally experience worsening of their other symptoms temporarily, due to fatigue. This is normal.
Fatigue affects each person living with MS differently. Symptoms may fluctuate over a daily, weekly and monthly basis and change in response to different activities. This can make fatigue challenging to manage, difficult to predict and complicated to explain to family, friends, colleagues and health professionals. Fortunately, there are lots of helpful and practical ways to help you manage your fatigue and minimise the effects on you.
Why do I suffer with fatigue?
Fatigue in MS is thought to be caused by different factors. In the literature, it is described as primary and secondary fatigue.
What is primary fatigue?
Primary fatigue describes the fatigue symptoms associated with the inflammatory processes occurring within the brain, spinal cord and nerves, due to the MS itself, essentially the tiredness you might feel just living with the changes going on in your body. When these plaques or blockages form in the brain, spinal cord or nerves your body tries to find ways around them, creating new pathways, this can also take up energy.
What is secondary fatigue?
Secondary fatigue is due to related factors of living with MS. These can include:
- Other MS Symptoms.
- Symptoms such as pain, muscle stiffness and muscle weakness can all affect how the body moves with MS. The additional physical effort can contribute to fatigue. Additionally, mood related symptoms such as depression, anxiety and stress may increase fatigue.
- Medication.
- Medications to treat MS and associated symptoms can have side effects. These may increase fatigue.
- Living with other health conditions.
- Other long term health conditions such as arthritis, cancer, stroke and diabetes also frequently report fatigue as a common symptom. Presence of these underlying conditions may further exacerbate symptoms of fatigue.
- Levels of physical activity.
- Prolonged periods of inactivity can lead to physical deconditioning. This can reduce the body’s physical reserves and the way it can cope with and manage symptoms of fatigue. Additionally, over-exerting yourself and doing something you don’t often do may have an impact on your energy levels the day after. Finding a balance between activity and rest is key.
- Lifestyle.
- Eating a poor diet, inadequate hydration, smoking, drinking alcohol and taking recreational drugs can all affect symptoms of fatigue.
- Local environment.
- Temperature, noise and lighting can affect how our body and mind feels. These factors may exacerbate symptoms of fatigue.
- Infection.
- Underlying infections can raise our body temperature and increase inflammatory activity. This process can increase symptoms of fatigue.
- Lack of sleep.
- Disturbed sleep because of pain, bladder disturbances or medication can affect our essential rest and symptoms of fatigue on subsequent days.
How do we measure fatigue?
We can measure fatigue using several tools. Visual analogue scales can be a simple way of measuring how we are feeling during the day, such as the two diagrams below.
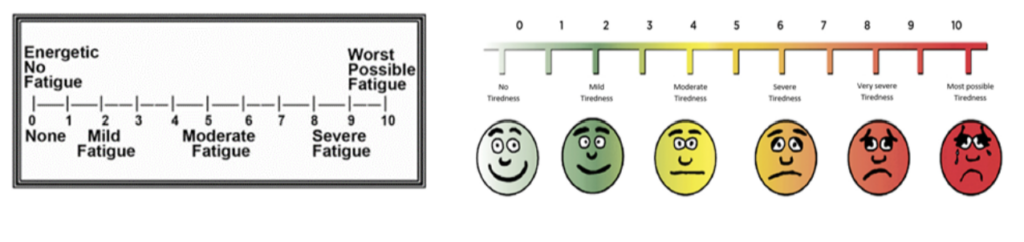
It can also be helpful to keep a fatigue diary, listing activities and scoring your tiredness on the scales above at the start and end of each day. This will give you a good idea of what impacts you the most.
How do we measure fatigue?
There are lots of simple ways that can help to manage fatigue. Considering these strategies into two main aspects may help. Firstly, we can manage fatigue by aiming to have the most energy available for your day.
How can I ensure I have the most energy available for my day?
- Getting a good night’s sleep
- A good quality night’s sleep can vary for everyone; however it is recommended that healthy adults need between 7-9 hours, sleep per night. Sleep is an essential part of a healthy lifestyle, allowing restoration of the mind and body. Sleep quality can be influenced by different factors, however having a consistent and relaxing sleep routine can help. This may include reading a book or listening to music, avoiding stimulants such as caffeine/tobacco, reducing screen time and being active during the day. Relaxation strategies may also help if it is difficult for you to fall asleep.
- Eating and drinking well
- Eating a well-balanced diet, rich in fresh fruit and vegetables can provide the body with essential fuel needed for daily life. This should include avoiding foods that are over-processed, high in sugar and in larger quantities, due to these foods leading to fluctuating energy levels over the day and more effort required to digest larger quantities. This coupled with regular and sufficient hydration during the day can assist in managing symptoms of fatigue.
- Exercise
- Regular physical activity and exercise is very important for helping to manage symptoms of fatigue. Exercise can improve muscle strength, balance, aerobic fitness, in addition to lifting mood and wellbeing. It can also optimise physical independence, reduce falls risk and assist the management of other symptoms e.g., pain, spasms. Physical activity and exercise are safe and strongly recommended for people living with MS. It is possible to do too much and should be increased gradually, listening to how your body feels, with time for rest. A physiotherapist can safely advise on the best source of physical activity. This may be water based (hydrotherapy), stretching, strengthening or a specific exercise regime.
- Symptomatic support for your MS
- Managing any MS symptoms or other factors which exacerbate your fatigue will be helpful. This may include treating underlying infections, maintaining a regular bowel habit, and addressing unwanted medication side effects. The involvement of MS Specialist nurses, GP’s, and other health professionals to address any areas of concern will be beneficial.
- Emotional support
- Our emotional and mental wellbeing is vital for helping to maintain our daily energy levels. Fatigue and mood related changes can commonly exist together and can sometimes be difficult to “untangle the two”. There are numerous resources and options for treating emotional and mental health symptoms. Successful treatment may lessen your fatigue. If your mood is affected by living with MS, seek help and support from your GP or MS nurse. They can talk through suitable treatment options such as talking therapies or medication.
How can I manage my energy in the most efficient way?
- Planning and pacing your day
- One of the main things you can do is plan and prioritise how you want to spend your energy. People living with fatigue can commonly experience a ‘boom and bust’ pattern to their activity. This includes trying to do lots of things when they have energy, subsequently running out of energy later in the day. Suggestions for managing this may include coordinating or delegating tasks to family, friends, and work colleagues, having a flexible daily routine and planning rest breaks. Additionally, consider how you may save energy during the day. Strategies such as online shopping, having external help with high energy tasks like cleaning and buying pre prepared food.
- Identifying how your fatigue behaves
- Keeping a fatigue diary may help you understand how your fatigue fluctuates and changes. This will enable you to make better decisions about how to structure your daily activities.
- Maintaining a good posture
- Undertaking tasks using a good sitting or standing posture can significantly assist with energy conservation, as it enables you to use your body most efficiently. Simply, sitting or standing tall, lifting, or moving items close to your body and bending your knees rather than your back or neck, can assist. Additionally, equipment such as having a height adjustable desk/chair or supportive chair can help. A Physiotherapist and an Occupational Therapist can both support optimising your posture for daily tasks. You are the best person to know how your fatigue responds to different factors and what your daily priorities are. Other health professionals that may be able to help you manage your fatigue include an Occupational Therapist, MS Specialist Nurse, a Physiotherapist and your GP. Finally, useful resources, information and support can be accessed via the MS Trust and MS Society Websites.